(MENAFN- Asia Times) SEOUL – Waiving intellectual property rights on Covid-19 vaccines will not upgrade global supply in the short term and could undermine the entire biopharmaceutical sector in the long term, a vaccine expert warned.
Dr. Jerome Kim, director-general of the International Vaccine Institute, which both develops non-commercial vaccines and supplies them to the developing world, urged related parties to carefully weigh the pros and cons of the step currently being mulled at the World Trade Organization (WTO) before adopting it.
While the proposal before the WTO looks, on the surface, to be a no-brainer in advancing global equality, if passed it would be – if Kim's analysis is correct – a disaster for all parties.
In the short term, it would not increase global supply. On the contrary, by introducing a new range of players and complicating current, finite supply chains, it would potentially reduce it.
Much of the manufacturing of current vaccines is, in fact, underway in developing countries with established industries. But contrary to a belief that local manufacturing in the Global South would enable cheaper domestic production, it would increase state healthcare costs, Kim says.
In the longer term, it would also reintroduce risks and inefficiencies to the sector that have not existed for over two decades. And, perhaps most perilously, it could stifle innovations in future disease control.
With the debate taking place against the Covid-19 carnage spreading across India and the sub-continent, Kim, who anticipates a major supply upturn this summer, urged cool-headed pragmatism.
'This will not solve the problem in the short term, so the time to discuss it is not in the heat of a pandemic when it is 'all hands on deck,' but when the lawyers can argue and when the diplomats can talk about it over coffee,' Kim said. 'In the longer term, it may build capacity that is not sustainable – and may frighten off the innovators next time.'

Dr. Jerome Kim, head of the International Vaccine Institute. Photo: IVI The case for waving patents The proposal to lift intellectual property protection, held by international pharmaceutical companies for Covid-19 vaccines, is rightly aimed at fairness. At present, the developed world – with notable exceptions such as Japan and South Korea – is racing ahead of the developing world in percentages of population vaccinated.
The arguments made by the representatives from South Africa and India at the WTO stated: 'Given this present context of global emergency, it is important for WTO Members to work together to ensure that intellectual property rights…. do not create barriers to the timely access to affordable medical products including vaccines. There are several reports about intellectual property rights hindering or potentially hindering timely provisioning of affordable medical products to the patients.'
On Wednesday, the India-South African proposal won a powerful supporter: President Joe Biden, who reversed the previous US position. Many in Biden's Democratic Party support the proposal.
And Washington could be said to have taken a hand in not just the approval of, but also the development of Covid-19 vaccines. Under 'Operation Warp Speed,' Washington promised billions of dollars to vaccine manufacturers, de-risking their R & D processes and accelerating rollouts.
The head of the World Health Organization (WHO), Tedros Adhanom Ghebreyesus, called Biden's support a 'monumental moment' which he said reflected, 'the wisdom and moral leadership of the United States.'
Discussions on the waiver are currently underway at the WTO, which oversees the Trade-Related Aspects of Intellectual Property Rights agreement. TRIPS is a key global standard for the oversight of intellectual property rights – copyrights, patents, trademarks and trade secrets.
While AstraZeneca has lost money on its vaccine, Pfizer is expected to make billions in profits , which has angered some. Pfizer earned US$3.5 billion in revenue from its Covid-19 vaccine in the first quarter of this year, representing nearly a quarter of its total revenue, Pfizer reported .
The vaccine, reports said, was, Pfizer's biggest source of revenue over the period. And while the pharmaceutical giant did not disclose how much profit it made from the vaccine, it has said that its profit margins on the vaccine would be in the high 20% range. That would translate into roughly $900 million in pretax vaccine profits in the first quarter.
Pharmaceutical company stock prices thus understandably dipped after Biden's statement.
To be sure, there is plentiful support for the IPR waiver.
There is a 'need to protect vulnerable populations' with 'cost-effective access' and the use of 'all production capacity, wherever it may be,' Kislaya Prasad, a research professor at the University of Maryland, said during a discussion program that aired on South Korea's Arirang TV on Friday.
Prasad further noted that the IP waiver initiative was being opposed by nations with strong pharmaceutical sectors.
France has joined the US and come out in favor of the proposal, and the EU Commission's president said on Thursday that she is open to the discussion. Germany, home to vaccine maker BioNTech, is leading the charge against.
A Berlin spokesperson on Thursday called IP protection 'a source of innovation,' adding that 'the limiting factor in vaccine manufacturing is production capacity and high-quality standards, not patents.'
Asia Times sought out a sectoral expert to gain his views on the issue.
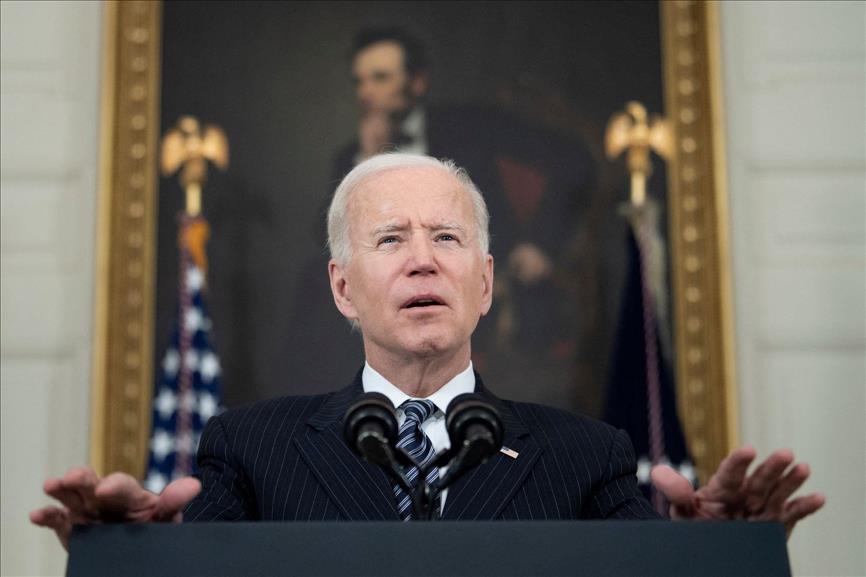
US President Joe Biden has hurled his weight behind a proposal to waive IPR on Covid vaccines. Photo: AFP Supply and production downside Kim could hardly be accused of being a rampant capitalist. The IVI is a not-for-profit organization that develops and distributes vaccines with limited commercial potential. As these products go to the global South, the IVI does not take (or enforce) IP protection on these vaccines.
'The IVI does believe in tech transfer: We transfer technologies to companies that are qualified and capable,' Kim made clear. However, the IVI's audit of such companies takes many months.
Amid the unprecedented scale of the Covid-19 pandemic, current production shortfalls are a result of supply bottlenecks. These will not be improved by lifting patent protection, he said.
'You don't want 206 countries making vaccines,' Kim warned.
An influx of new entrants – companies and countries with little or no experience in vaccine manufacturing – would only complicate supply chains. And supply chains extend beyond vaccines per se.
'Medical glass is a particular glass, and the stoppers for the vials, the needles, and all these other things are going to be put under pressure by additional suppliers coming online,' Kim said. 'There is a finite number of suppliers that can make these things.'
Moreover, new entrants – for example, drug companies – largely lack necessary expertise.
'I can give you the formula but you will still have to make it, and there is a world of difference between a drug, which is chemical, and a vaccine, which is biological,' he said. 'A vaccine is very difficult to duplicate – even if its patent runs out.'
A further complication is that biologically based vaccines require biological materials that often have technical variabilities. This requires onerous oversight to enable batch consistency.

A production line for the Sinovac vaccine in Beijing. Photo: Xinhua
'It can be 50,000 steps that have to be quality controlled,' Kim said. 'And that process has to be done the same way, every single time,' Kim said.
These are problems even for highly experienced companies and manufacturers at the top of the feeding chain.
'We knew from the start that the first nine months [of Covid-19 vaccination rollout] was going to be rough,' Kim said. 'There will be glitches expanding supply, a batch may fail or a batch can be contaminated – and these things happen to companies that make vaccines.'
It is not only factories in the world's richest nations that are producing vaccines at present: first-world vaccine developers customarily outsource much of their manufacturing. Indeed, two of the largest vaccine manufacturing centers are, in fact, in two of the most heavily impacted countries.
'For global vaccines, the key makers are in Brazil, India, Indonesia and South Korea,' Kim said. Vaccine makers 'can trust the companies in these countries.'
According to Reuters , some 200 technology transfer agreements have already been made around the world.
A key reason why supply to the global COVAX initiative – which delivers vaccines to the developing world at reduced or no cost – is behind schedule is because an embattled New Delhi has halted all exports of the AstraZeneca vaccine made domestically. And of the four countries mentioned, India is responsible for the largest share of manufacturing – approximately 60%.
The issue is not just about efficient companies. National regulatory authorities in these countries have built up the necessary skills, which is not the case elsewhere. 'You don't want regulators of a vaccine industry that have never done it before and can't do it correctly,' he said.
The amount of paperwork required to get a vaccine through a global-standard approval process is enough to fill a truck, he noted.

A health worker loads a syringe with the Moderna vaccine. Photo: Apu GOMES / AFP) Increased costs, reduced efficiencies Moreover – and perhaps contrary to the conventional wisdom – releasing vaccine IP, thereby allowing current vaccines to be produced in developing countries, would not reduce costs for those countries. On the contrary, not only would it increase those costs, it could feasibly turn the sectoral clock back to a less efficient, more expensive past.
'From the 1950s to the late 1990s, more companies used to make their own vaccines,' Kim explained. 'State-owned companies made them, but they were expensive and inefficient, so it was better for a country to buy from one of the big manufacturers, or from an Indian manufacturer.'
The issue boils down to costs and quality – and related competencies and efficiencies. 'If you were a small country and want to make your own vaccine, can you compete with companies that are making hundreds of millions of doses?' he asked.
While Kim's organization does not legally protect the IP of its own vaccines – produced largely to deal with diseases that are not commercially viable for the major players to combat – he sympathized with the needs of the big players that spend billions on R & D.
Most particularly, the release of their IP would remove the veil from some deep science, for current-generation Covid-19 vaccines are built on long-in-development 'platform' vaccines that also have the potential to deal with a wider range of diseases.
Calling it 'the secret formula,' Kim said. 'the liquid nano-particle is something biotech will not only use for Covid, but also, for, say, a cancer vaccine. Take that away and you are depriving a company of possibly billions.'
This is why he sympathizes with Berlin and the Big Pharma lobby.
'They have a point,' he said. 'Companies make this willingly and will make billions this year, but if you tell them, 'We are not going to allow you to prosecute IP violations,' what is Pfizer, for example, going to say the next time there is a big pandemic?'

Staff deliver food to patients at the temporary hospital for Covid-19 patients, organized in the Lenexpo exhibition complex, where patients suffering from coronavirus disease are treated in St Petersburg, Russia. Photo: AFP/Alexei Danichev/SputnikMENAFN07052021000159011032ID1102045776